Oxygenation intervals have a peculiar regulatory, normalising role. When hypoxic exposure is repeated multiple times, these oxygenation intervals attenuate hypoxia intensity to optimise conditions required for the development of long-term adaptation and prevent overdosing hypoxia.
During the re-oxygenation phase, induction of mild oxidative stress takes place within the cell, leading to the initiation of adaptive reactions cascade. The end result is both hypoxia and hyperoxia-induced activation of numerous transcription factors (NF-kB, АР-1, HIF-1-alpha, HIF-3-alpha) which induce protective proteins, such as antioxidative enzymes, HSP, FeRP, growth factors, and repair enzymes. Therefore, the cells become saturated with protective molecules. Induction of reactive oxygen species (ROS) synthesis depends on the degree of hypoxia achieved. At the same time, the use of breathing mixtures with oxygen concentrations below 10% is very likely to produce adverse effects even if applied for a very short period of time.
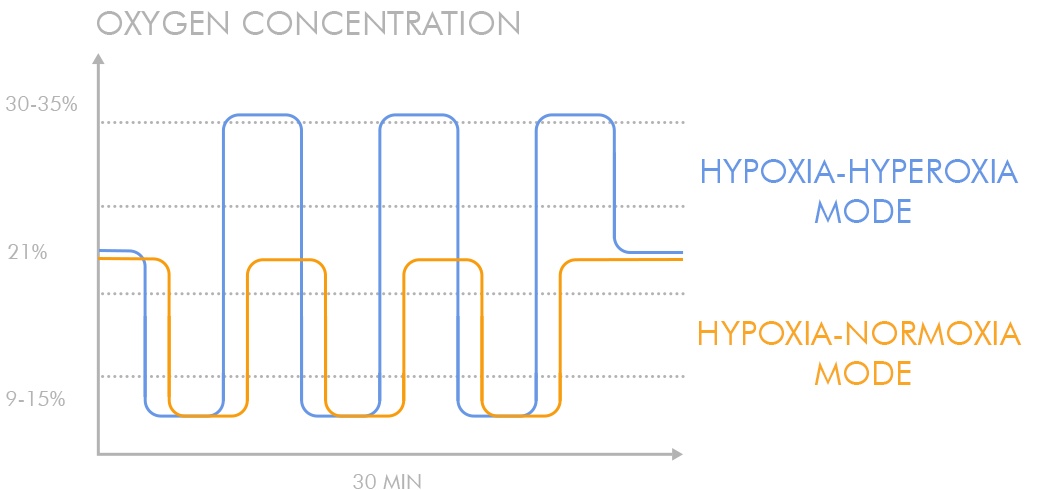
The replacement of normoxia periods by their hyperoxic (from 30% to 40% O2) counterparts significantly increases the treatment factor amplitude resulting in a stronger ROS signal without the need to utilise more intense and risky hypoxia.
Besides, faster patient re-oxygenation leads to a reduction of therapeutic session length.